Watchdogs say unemployment fraud likely topped $191 billion
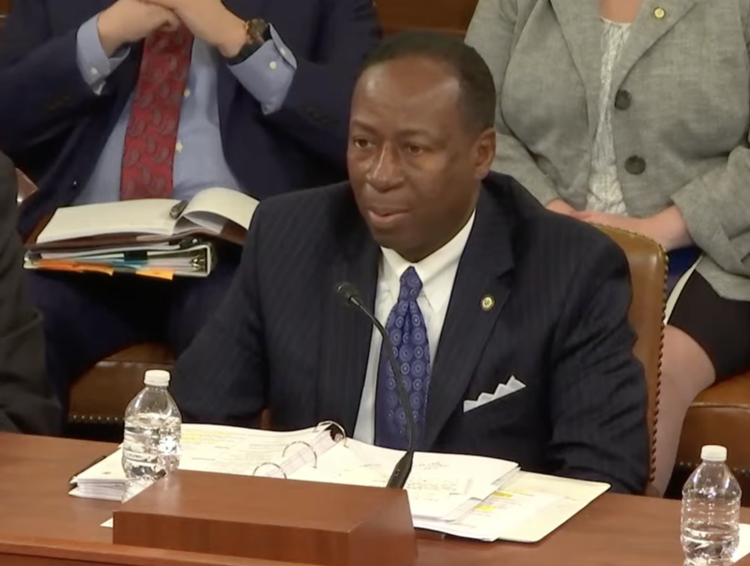
Slightly more than $1 out of every $5 distributed in unemployment insurance payments during the pandemic could have been improper, mostly fraud. Larry Turner, the inspector general for the U.S. Department of Labor, said Wednesday that of the more than $888 billion in total federal and state unemployment insurance benefits distributed during the pandemic, at least $191 billion could have been improper payments, “with a significant portion attributable to fraud.” Turner told members of the House Ways and Means Committee during a hearing. That’s up from a previous estimate of $163 billion. “The reliance solely on claimant self-certifications without evidence of eligibility and wages during the program’s first nine months rendered the Pandemic Unemployment Assistance program extremely susceptible to fraud,” he said. The Pandemic Unemployment Assistance program provided unemployment insurance benefits to people who were traditionally not eligible for benefits, including gig workers, self-employed workers, and independent contractors. States administer unemployment insurance with oversight from the U.S. Department of Labor. In place for more than eight decades, the joint state-federal program serves as a safety net for people who lose their job through no fault of their own. When the pandemic hit, a combination of factors resulted in a spike in improper payments and fraud. A 2022 audit found that fraudulent claims were paid 60.5% of the time from March 28, 2020, to September 30, 2020. “This created multiple high-reward targets where an individual could make a fraudulent claim with relatively low risk of being caught,” Turner said. “For example, as time went on, one fraudster could have been issued several UI debit cards, with tens of thousands of dollars on each card.” As an example, Turner cited a person who filed a claim from a three-bedroom house that was the shared location for 90 other claims. The same person also shared a flagged email address with 145 other claims. In total, that person was connected to 235 other claims in three states and got benefits on 87 of those claims, all filed in California, for a total of $1,569,762. California stopped payment 164 days after the initial payment when officials were unable to verify the person’s identity, according to that 2022 audit. Part of the problem was the nature of the crisis. The pandemic and governments’ response to it put millions of people out of work in a matter of weeks. Unemployment levels rose to historic levels. On March 14, 2020, the Department of Labor reported 282,000 initial unemployment claims. Within weeks, initial claims rose to 10 times pre-pandemic levels, “far higher than state systems were designed to handle,” Turner said in written testimony. Within five months, the Department of Labor reported 57.4 million initial claims, the largest increase since the agency began tracking unemployment insurance data in 1967. Problems with the unemployment insurance program predated the pandemic. Turner said the program had among the highest improper payment rates in the federal government. It had been above 10% for 15 of the previous 19 years. In the last two years, the agency has estimated an improper payment rate of 18.71% and 21.52%, respectively. Comptroller General of the United States Gene Dodaro told the committee that some improvements have been made to prevent fraud, but more remains to be done. “I think we’re slightly better prepared, but not fully prepared for the next crisis,” he said. “A number of our recommendations at the Labor Department have been not fully implemented yet. I think states are trying to make improvements – there have been some improvements that have been made, but they’ve all been ad hoc. There hasn’t been a systematic approach to doing this.” He said while the government should work to recover as much fraud as it can, prevention would go further. “The only way to effectively deal with this is to prevent it up front,” Dodaro said. Michael Horowitz, chairman of the Pandemic Response Accountability Committee, told the House Ways and Means Committee that the fraud was not limited to U.S. residents. “One of the biggest challenges we have is following the fraud through overseas gang activity and fraudsters,” Horowitz said. “The Secret Service has reported that they’ve seen that occur through entities in Nigeria, China, Russia. That will be our biggest challenge.” U.S. Rep. Vern Buchanan, R-Florida, asked for an estimate of how much that type of fraud cost U.S. taxpayers. Horowitz said no such estimate was available. “That’s among the hardest fraud to find, track, and figure out,” he said. “Because it is through overseas networks … the process is very challenging.” Republished with the permission of The Center Square.
Gary Palmer demands cost analysis of Build Back Better legislation
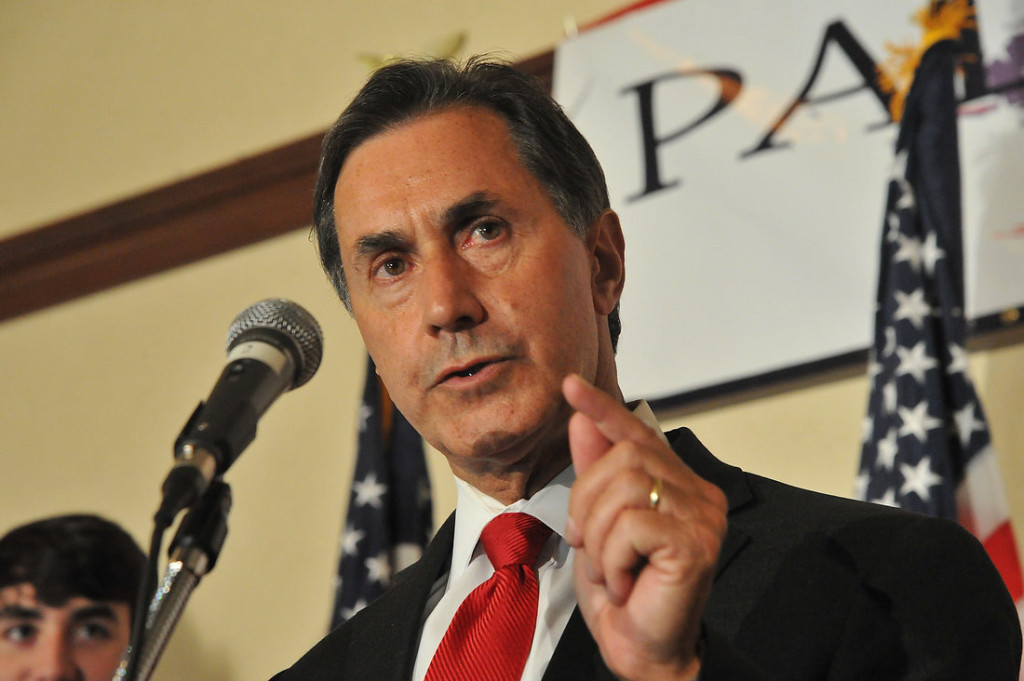
Congressman Gary Palmer and several colleagues have sent a letter to Congressional Budget Office Director Phillip Swagel. The group has requested cost analysis of the Democrats’ Build Back Better legislation. In a press release, Palmer stated, “The nation will have to build back from the brink of bankruptcy, should this legislation ever become law. Although the Democrats are pretending to scale back on a number of the unwarranted programs in it, we have no idea what the true price tag is for these policies that would fundamentally undermine our Republic and move us one step closer to socialism.” According to a recent article from the House Committee on the Budget Chairman John Yarmuth, the Build Back Better Act “aims to make an investment of $1.75 trillion in family care, health care, and combatting the climate crisis.” However, Palmer argues that the initiative will cost more than what is being stated. “I have seen more than one or two budget gimmicks during my time in Congress, and this package is full of them,” Palmer continued. “For instance, the legislation partially funds programs and pretends they will come to an end, even though the clear intention is to make them permanent. This is why we have requested that the CBO Director conduct a true analysis, so that Congress and the American people have a real understanding of just how much this monstrosity will cost. Independent groups have consistently said this bill is not paid for and will increase the deficit. This analysis will expose all of the bill’s budget gimmicks and hopefully end this misleading effort to run our country over the fiscal cliff.” The letter states, “H.R. 5376, as it is currently drafted, contains cherry-picked program expirations and phase-out periods that are meant to circumvent congressional scoring procedures. These provisions are disingenuously meant to hide the true costs of these policies and their burden on Americans today and for generations to come. It is of paramount importance that before Congress collectively acts on this legislation, it has an accurate understanding of what the effects of this legislation would be if its policies became permanent law.” The letter was also signed by Reps. Vern Buchanan, Greg Steube, Pete Stauber, Mariannette Miller-Meeks, Jack Bergman, David Rouzer, Tracey Mann, Mary E. Miller, Tedd Budd, Markwayne Mullin, Jody Hice, Eric Crawford, David McKinley, and Andy Biggs.
Terri Sewell introduces bipartisan bill to ensure patients have access to home infusion services

Rep. Terri Sewell joined legislators Fred Upton, Debbie Dingell, and Vern Buchanan to introduce H.R. 5067, the Preserving Patient Access to Home Infusion Act. This bipartisan bill would ensure patients with serious viral and fungal infections, heart failure, immune diseases, cancer, and other conditions receive IV medications they need while at home. Companion legislation was introduced in the U.S. Senate by Mark Warner and Tim Scott. Sewell stated, “Countless Alabamians, especially those in rural communities, rely on home infusion services for life-saving care. With the risks posed by the COVID-19 pandemic, it has never been more critical to ensure that patients continue to receive this care safely in their homes. I’m so proud to introduce this bipartisan bill and urge my colleagues on both sides of the aisle to give it their full support.” Rep. Upton commented, “While the COVID-19 pandemic certainly took so much from so many, it also gave us the opportunity to rethink the way that we care for the most vulnerable among us. Home infusion, in particular, is a perfect example of how we can bring healthcare services into folks’ homes while keeping both patients, their families, and medical professionals safe and healthy. I am proud to co-sponsor this important legislation and will continue to work with my colleagues on both sides of the aisle to expand access to quality, affordable healthcare.” “As we have learned from the coronavirus pandemic, home health services have proven to be invaluable for seniors in my district and across the country,” said Rep. Buchanan. “The aptly-named Preserving Patient Access to Home Infusion Act will ensure that Medicare recipients are able to continue to receive life-saving drugs in a safe and effective way from the comfort of their own home.” Patients with serious infections, cancer, heart failure, immune system diseases, and other conditions who need medications such as IV therapies can receive these medications in their homes rather than hospitals or nursing homes. Research shows that up to 95% of patients would prefer receiving their infusions at home. Congress included provisions for this in the 21st Century Cures Act and the Bipartisan Budget Act of 2018. However, the Centers for Medicare and Medicaid Services (CMS) didn’t implement the benefit properly. They required a nurse to be physically present in the patient’s home for providers to be reimbursed. As a result, provider participation has dropped sharply, and beneficiaries have experienced reduced access to home infusion over the last several years. The act provides technical clarifications that will remove the physical presence requirement, ensuring payment regardless of whether a health care professional is present in the patient’s home. The bill will save $93 million over 10 years. “Home-based infusion services stand out as high-value resources that improve patient quality of life and add capacity to the health care system while providing cost-savings for the Medicare program,” said NHIA President and CEO Connie Sullivan. “Passage of the Preserving Patient Access to Home Infusion Act is critical to ensuring the Medicare program maintains access to home infusion, allowing beneficiaries to safely receive treatment in the setting they overwhelmingly prefer: their homes.” “Providing IV medications in patients’ homes allows individuals to receive their treatments without major sacrifices in their quality of life and without having to rely on transportation to travel to a facility for their treatments,” said Logan Davis, MBA of Vital Care InfusionServices. “This legislation will ensure that the Medicare home infusion therapy benefit is accessible to patients, including many who are located in Alabama’s rural or historically underserved communities.”

